Bedwetting is a common issue many families face, but it can be particularly challenging for children with autism and their parents. By understanding how prevalent bedwetting is among autistic children and recognising the underlying causes, we can raise awareness and provide better support for these families.
Common Causes of Bedwetting in Autistic Children
Awareness of Bodily Cues
Children with autism often struggle to recognise bodily cues that indicate the need to use the toilet. This lack of awareness can lead to accidents during both the day and night. Teaching children to identify these cues can be a gradual process, requiring patience and consistent reinforcement. Visual aids, such as pictures and social stories, can be effective tools in helping autistic children understand and respond to their bodily signals.
Daytime Toileting Challenges
It's crucial to establish effective daytime toileting routines before addressing nighttime bedwetting. Issues like stool withholding, constipation, and infrequent drinking can impact bladder control and contribute to bedwetting. These factors affect all children, not just those with autism. Creating a regular schedule for bathroom breaks, encouraging sufficient hydration, and addressing constipation through diet and medical advice are essential steps in managing daytime toileting issues. Additionally, using positive reinforcement and rewards for successful bathroom visits can motivate children to develop better habits.
Communication Difficulties
Autistic children may have difficulty expressing their need to use the bathroom or understanding toileting instructions. This communication barrier can result in accidents and frustration for both the child and the parents. Parents can use visual schedules and communication boards to aid in conveying the steps of the toileting process. Speech and language therapists can also provide valuable strategies to improve communication skills related to toileting.
Irregular Sleep Patterns
Many autistic children experience irregular sleep patterns or insomnia. These sleep disruptions can prevent children from waking up to use the bathroom during the night, leading to bedwetting incidents. Establishing a consistent bedtime routine and creating a calming sleep environment can help improve sleep quality. Techniques such as using white noise machines, blackout curtains, and weighted blankets may be beneficial. Consulting with a sleep specialist or pediatrician for further guidance on managing sleep disorders is also advisable.
Stress and Anxiety
Changes in routine, transitions, or other stressors can significantly impact autistic children, causing increased anxiety. This anxiety can contribute to bedwetting as the child may struggle to cope with these changes. Identifying and addressing sources of stress is crucial. Parents can use calming techniques such as deep breathing exercises, sensory activities, and creating a predictable daily schedule to help reduce anxiety. In some cases, working with a therapist specialising in autism can provide additional support in managing stress.
Developmental Delays
Children with autism often experience delays in reaching developmental milestones, including nighttime bladder control. These delays mean that achieving consistent dry nights may take longer compared to neurotypical children. Understanding and accepting these delays is important for parents. Customised toilet training programs that consider the child's developmental level and individual needs can be more effective. Occupational therapists can assist in developing tailored strategies to support the child's progress in achieving bladder control.
Here are some strategies to help manage and reduce bedwetting incidents with Patience and Understanding:
Establish a Consistent Routine
Create a regular toileting schedule during the day and before bedtime. Consistency can help the child develop better bladder control. Encourage bathroom visits at regular intervals, such as after meals and before bedtime. Using a timer or alarm can serve as a reminder for both the child and parents.
Use Visual Aids
Utilise visual aids and social stories to help the child understand the steps involved in using the toilet. Visual schedules showing the sequence of toileting tasks can be displayed in the bathroom. Social stories, which are short narratives describing toileting routines, can be read regularly to reinforce the process.
Encourage Hydration
Ensure the child drinks adequate fluids during the day but limit excessive drinking before bedtime. Monitoring fluid intake can help establish a healthy balance, preventing both dehydration and overloading the bladder before sleep. Offering water-rich fruits and vegetables can also contribute to hydration without excessive liquid intake.
Manage Constipation
Address any constipation issues by encouraging a healthy diet rich in fiber and regular physical activity. It's important to address constipation as it is the number one cause of bedwetting due to a full bowel putting pressure on the bladder. Foods such as fruits, vegetables, whole grains, and plenty of water can help maintain regular bowel movements. Parents may also consult with a pediatrician for guidance on using fiber supplements or stool softeners if necessary.
Create a Calm Environment
Minimise stress and anxiety by maintaining a predictable routine and providing a calming bedtime environment. Incorporate calming activities before bed, such as reading a book, listening to soothing music, or engaging in gentle sensory activities. Creating a quiet and comfortable sleep space can promote better rest and reduce nighttime awakenings.
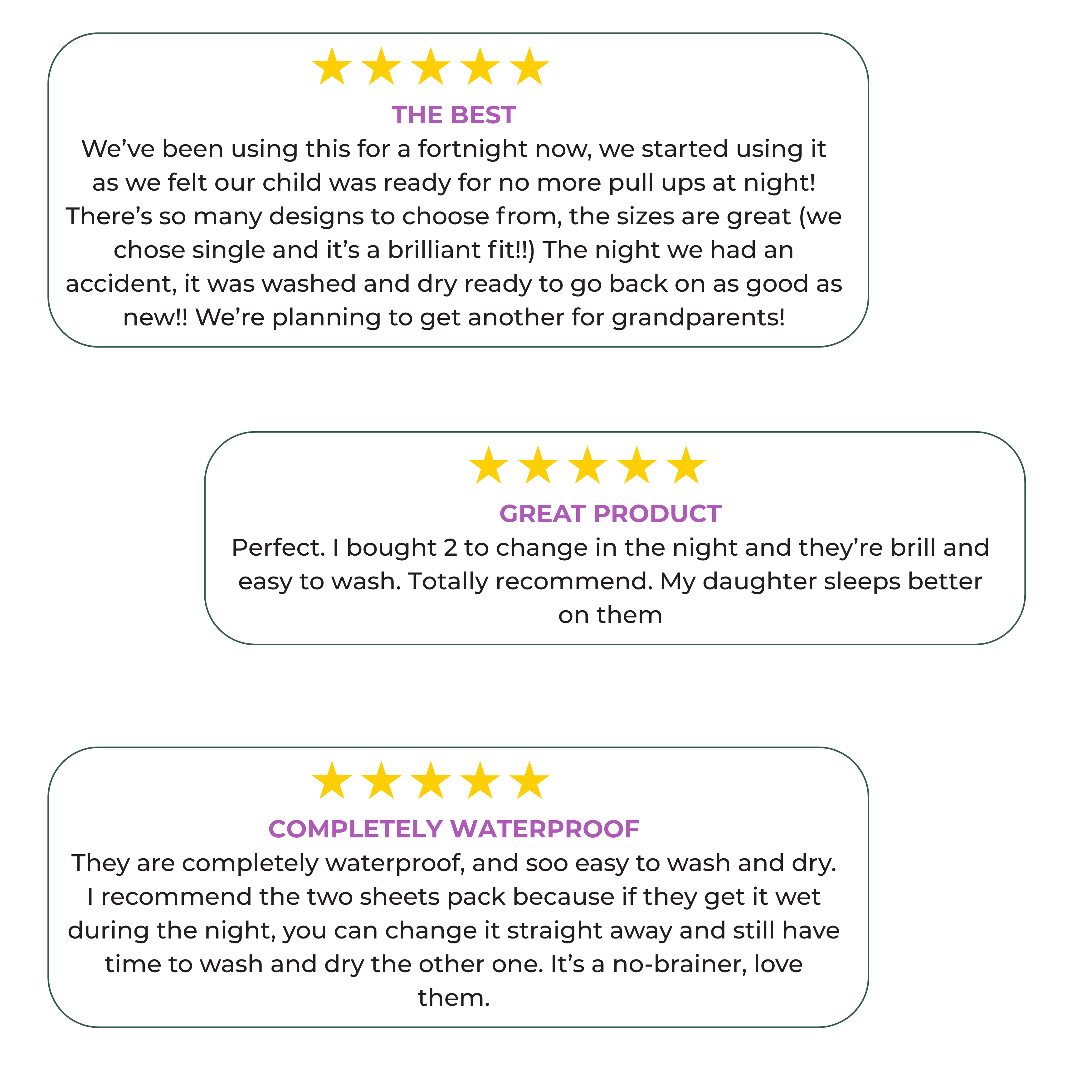
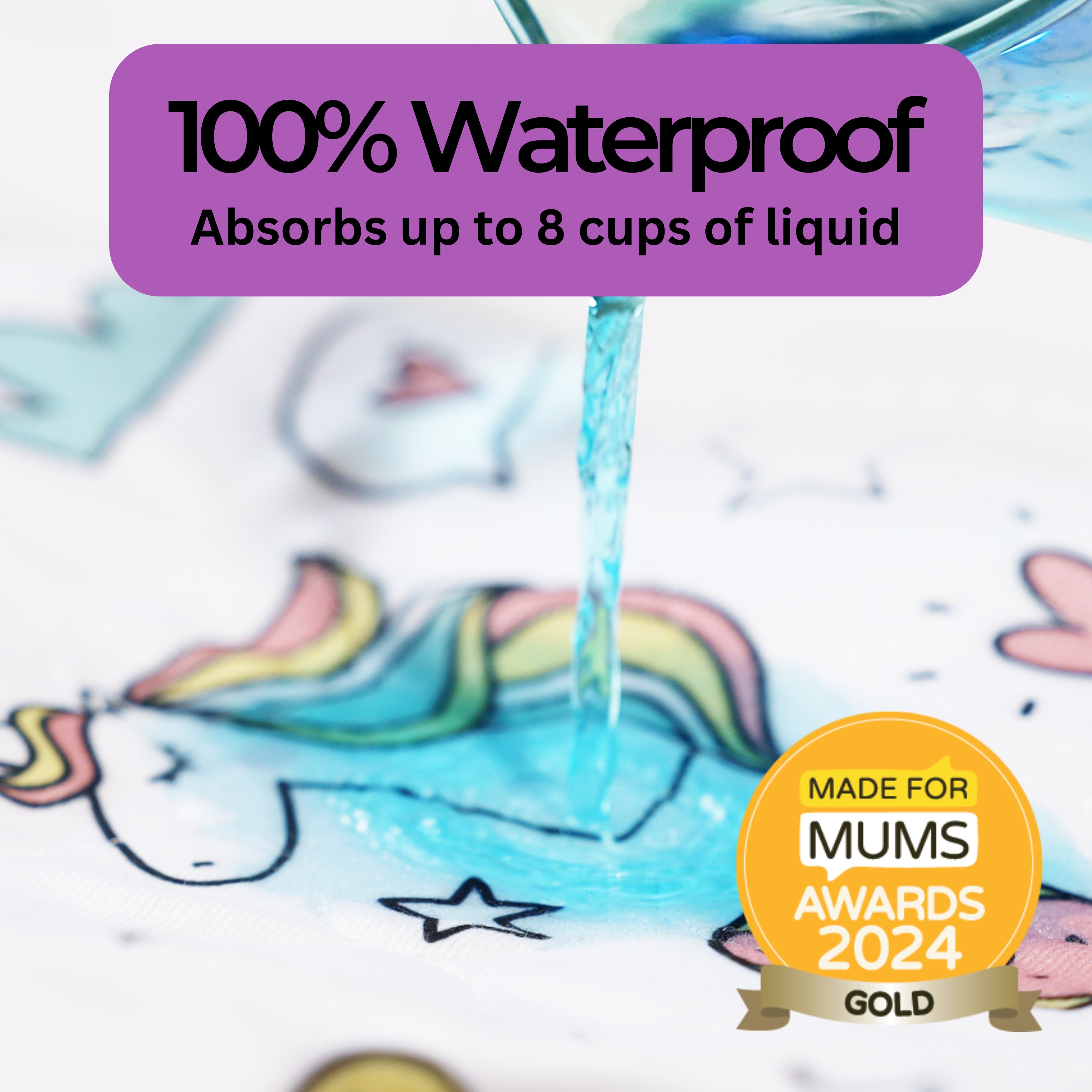
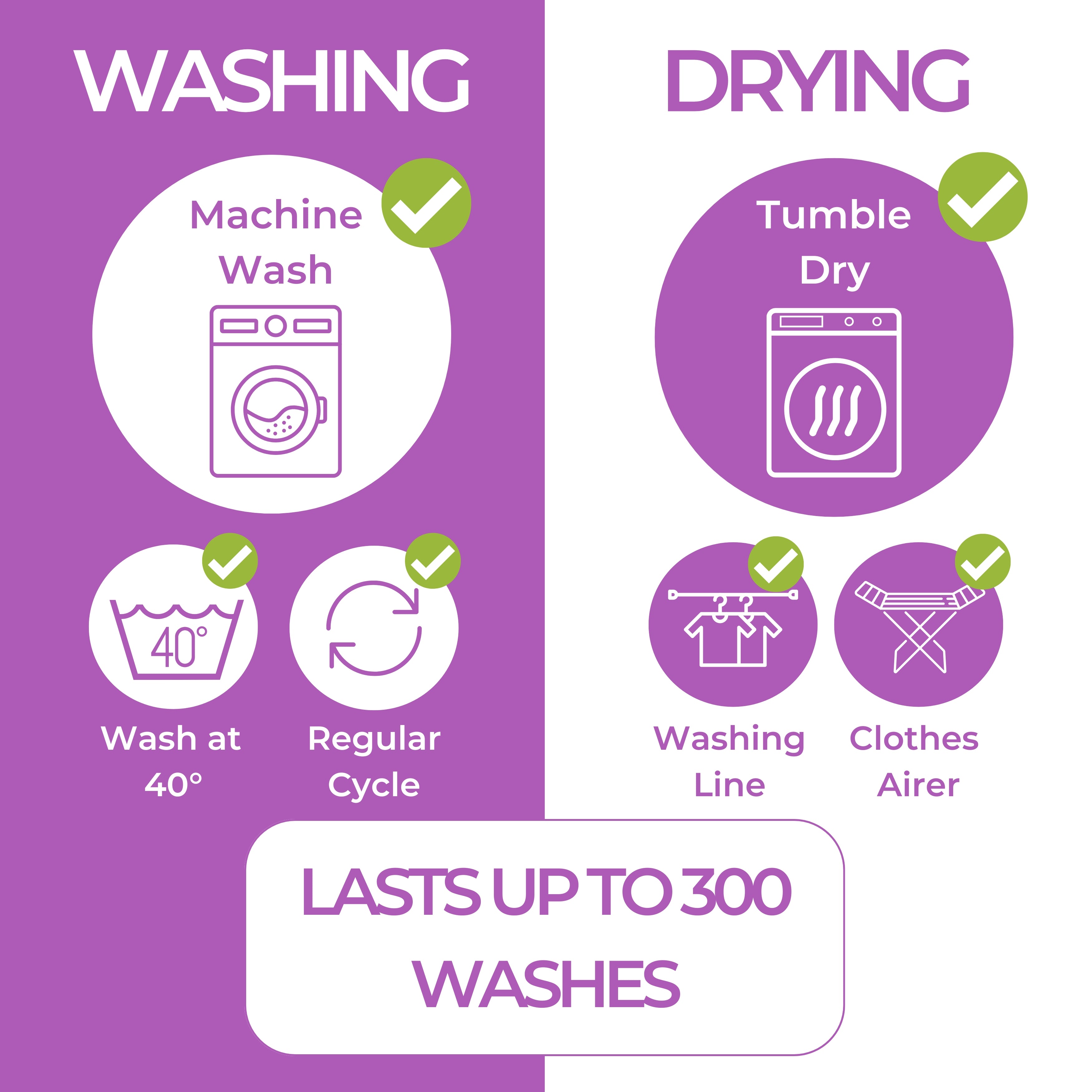
Use Protective Bedding
Consider using waterproof mattress protectors and bed pads such as Hygge Sheets to manage accidents and make cleanup easier. Protective bedding can prevent damage to the mattress and reduce the stress of frequent bed changes. Having spare sheets and pyjamas readily available can also simplify nighttime disruptions.
Seeking Professional Help
If you are concerned about your child's bedwetting, it's essential to consult your healthcare provider, such as your GP or pediatrician. Medical professionals can conduct assessments to rule out urinary tract infections, sleep disorders, or other conditions that may contribute to bedwetting.
Community Support and Resources
Connecting with other parents and support groups can provide valuable insights and emotional support. Sharing experiences with families facing similar challenges can reduce feelings of isolation and offer practical advice. Online forums, local support groups, and organisations dedicated to autism and childhood development can be excellent resources.
Educating and Empowering Families
By raising awareness of the common causes of bedwetting in autistic children and offering practical solutions, we can support families through this challenging time. Educating parents and caregivers about the nuances of bedwetting in children with autism empowers them to implement effective strategies and seek appropriate help. Understanding that patience and empathy are crucial in addressing bedwetting can lead to more positive outcomes.
Conclusion
Bedwetting in children with autism can be a complex issue that requires a compassionate and informed approach. By addressing the underlying causes, establishing consistent routines, and seeking professional guidance, families can navigate this challenge with greater ease. Remember, patience and understanding are key to helping your child achieve nighttime dryness, fostering a supportive and nurturing environment for their growth and development.