Many children under the age of five wet the bed. However, after this age, it is classed as a medical condition called nocturnal enuresis.
If your child is over five and still bedwetting, please don’t worry! My eldest daughter was over five when she became dry at night, and my youngest is also five and not yet dry. This post is here to help you. We explore the reasons for continued bedwetting and some of the strategies you can use to reduce it over time. Here’s everything you need to know.
Why Do Children Wet the Bed at Night?
Bedwetting isn't a child’s fault or a serious medical condition. However, many parents become more conscious of it as their child gets older, as they don’t want it to impact their child’s self-esteem.
Bedwetting can occur for several biological reasons. Some children have small bladders that don’t hold all the urine produced by their kidneys at night. Eventually, the bladder fills and releases its contents automatically.
Other children’s bladders fail to properly signal the need to go to the toilet to the brain at night. As a result, the child doesn’t wake up and urinates in their sleep.
Finally, some children produce too much urine at night, either due to drinking a lot before bed or hormonal imbalances.
While there are many reasons for bedwetting, it is treatable using evidence-based approaches. These strategies address the root cause of bedwetting and help children achieve drier nights.
Bedwetting doesn’t mean a child is being naughty. It is a natural part of growing up. Some children take longer than others to stay dry at night, which can be concerning for parents. However, every child is different, and it’s important not to compare them to others.
If your child has a bedwetting incident, be supportive. Don’t blame or punish them for what happened.
Understanding Nighttime Potty Training
Sometimes, health complications contribute to bedwetting. Therefore, it’s important to rule these out with a healthcare provider first.
For example, constipation can press on the bladder and cause increased urgency. Urinary tract infections and Type II diabetes (although rare in young children) can also increase the risk of bedwetting.
Sometimes, bedwetting occurs due to external factors such as stress. For instance, starting a new school can disrupt bladder-brain signalling at night. Anxiety can also increase vasopressin production, a hormone that slows urine production.
Nighttime potty training involves using various strategies to help a child stay dry when none of the above conditions apply.
If your child suddenly starts bedwetting after being dry for more than six months, speak to a doctor or paediatrician. Identifying the cause is key to successful treatment.
Overnight Potty Training: Mastering the Process
Here are some strategies to help prevent bedwetting:
1. Get a Bladder and Bowel Assessment
The first step is to take your child for a bladder and bowel assessment, as recommended by NICE guidelines for children over five who wet the bed. This helps medical professionals identify any underlying issues.
In the UK, some GPs may turn children away until they are seven, despite the guideline recommending age five. I discussed this on our Instagram here. If your GP is unhelpful, there are other routes to support. We have compiled a list of trusted experts and organisations, including private incontinence consultants and the ERIC charity, here. Your school nurse may also be a helpful resource.
2. Use a Bedwetting Alarm
Bedwetting alarms help children with poor nighttime arousal by waking them when they begin to urinate. These devices train the brain to associate the sensation of needing to wee with waking up.
If a GP finds no medical issues after an assessment, they may provide a bedwetting alarm.
How to Use Bedwetting Alarms Effectively:
-
Alarms take time to work. Most children need at least a month of consistent use.
-
Some parents sleep in the same room initially to support their child’s response.
-
Show your child how the alarm works before using it at night to avoid distress.
You’ll know the alarm is working when your child starts having dry nights more frequently. If there is no progress after three months, take a break and try again later.
3. Get Bedwetting Medication
If alarms don’t work, a doctor may prescribe medication. The most common option is Desmopressin, which increases vasopressin levels and reduces nighttime urine production.
4. Use Special Tactics When Travelling
Bedwetting can be challenging when travelling, especially if your child is staying elsewhere. Strategies include:
-
Talking to a doctor about Desmopressin for short-term use.
-
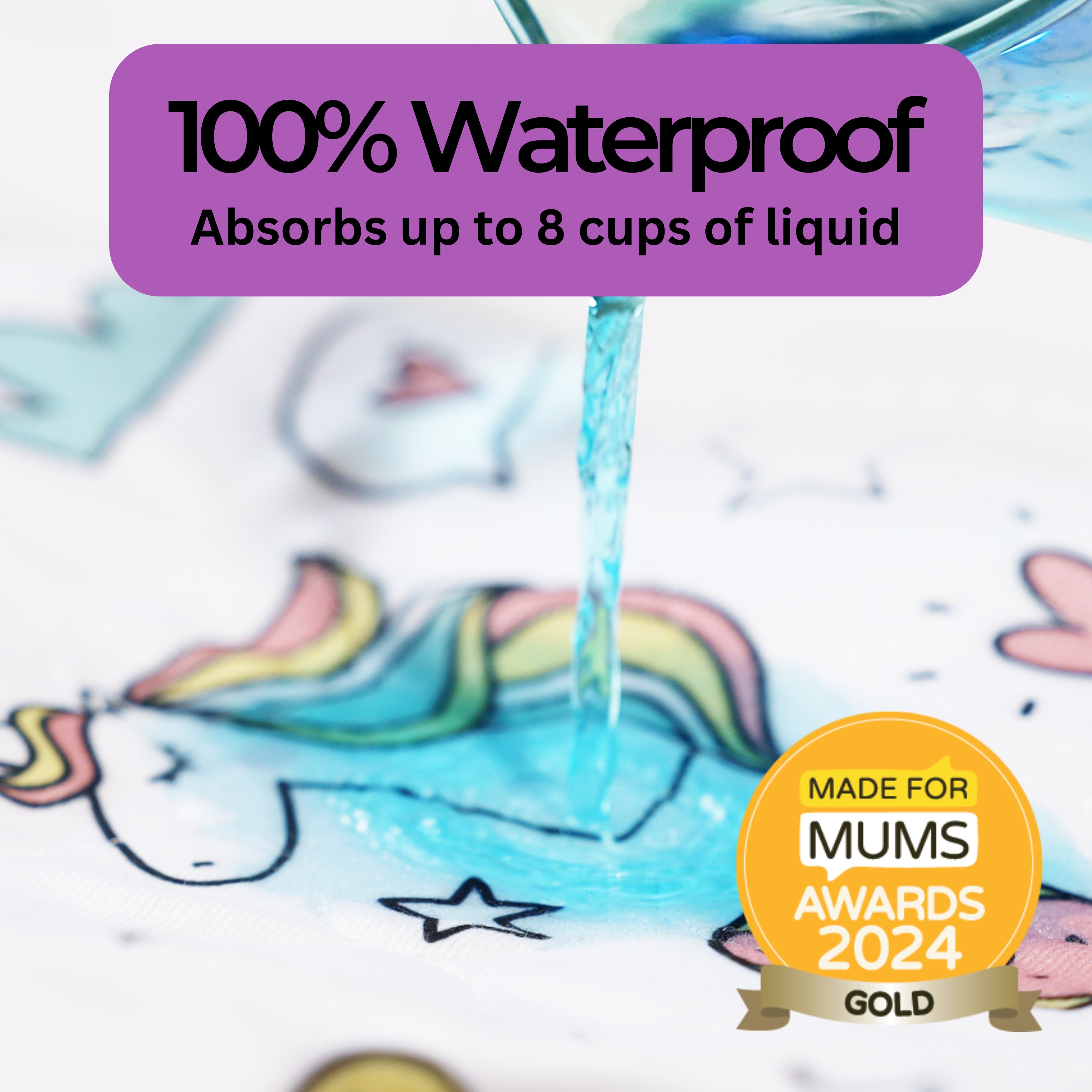
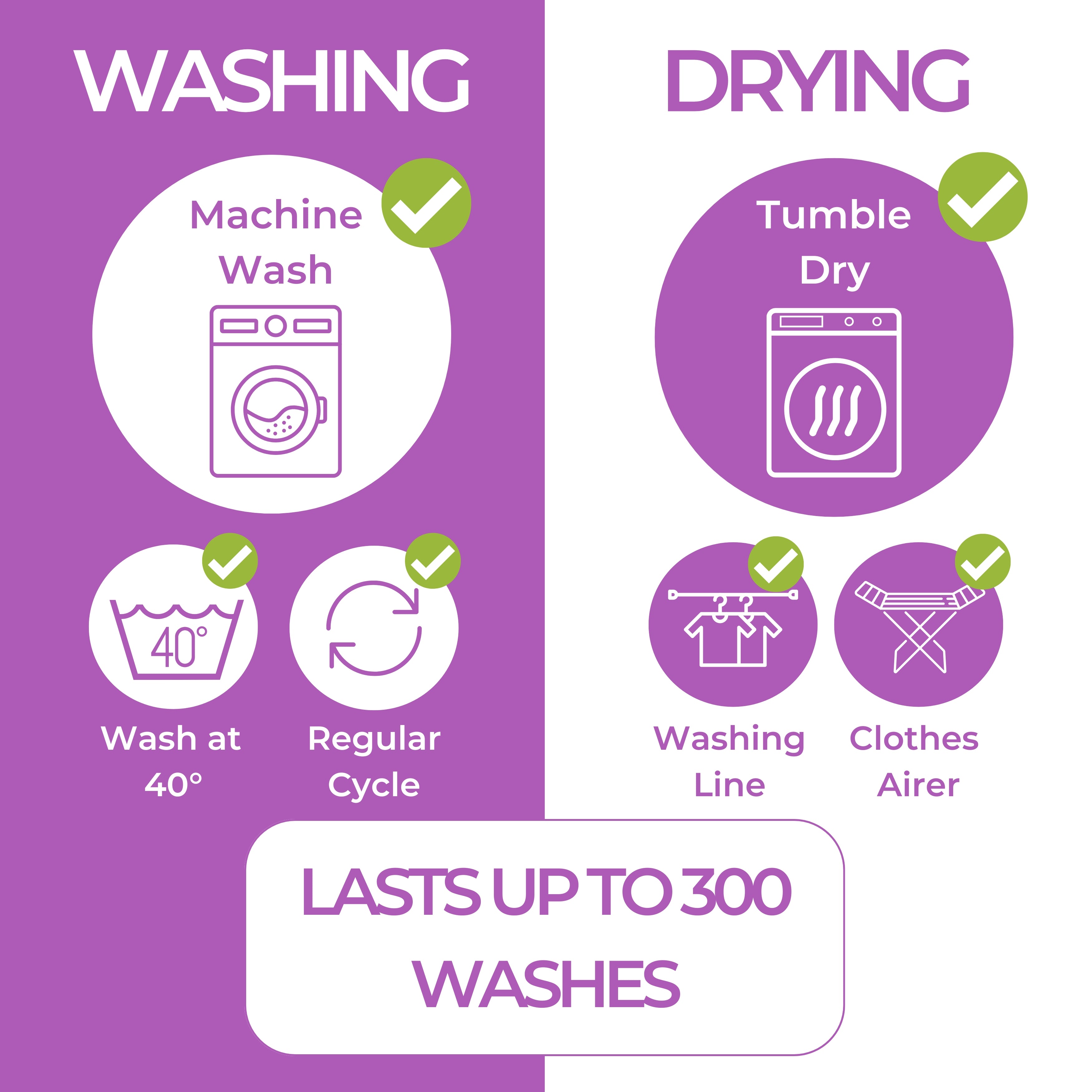
Packing a waterproof sheet for mattress protection.
-
Bringing extra bedding and clothing in case of accidents.
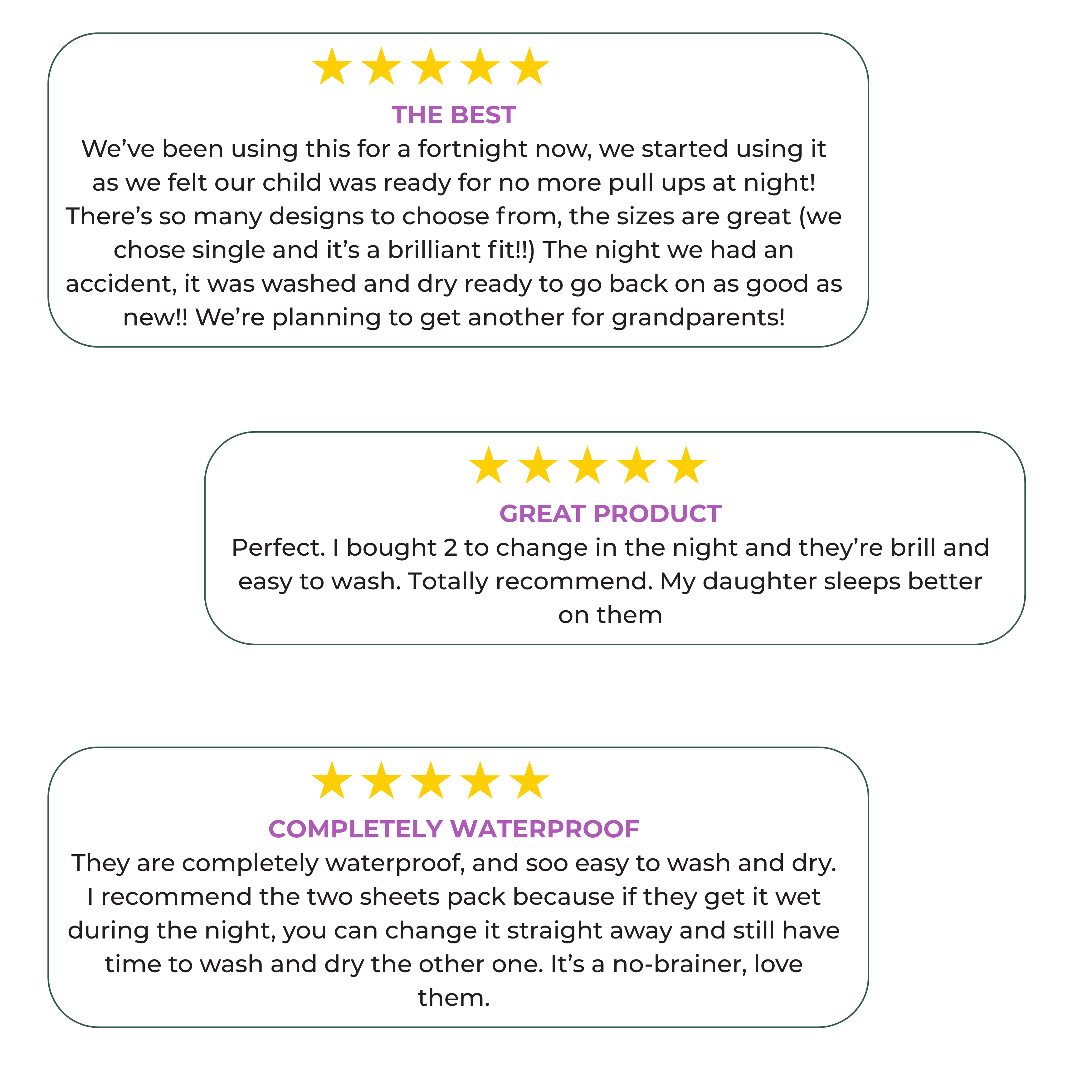
Many of our customers take a Hygge Sheet Mattress Protector on holiday. Personally, I don’t know what I’d do without it!
Top Tips for Potty Training at Night
-
Check for daytime bladder issues such as overactive bladder or constipation.
-
Ensure your child empties their bladder before bed. A double void (weeing twice before bed) can be helpful.
-
For boys, encourage sitting down to wee before bed. More on that here.
-
If your child sleeps in a bunk bed, move them to the bottom bunk for easier bed changes.
-
Reassure your child that they will eventually achieve dry nights.
-
Encourage hydration throughout the day and limit fluids an hour before bed.
Potty Training Your Toddler at Night
For children under five, similar strategies apply. Research suggests children who can nap for two or more hours without wetting are more likely to stay dry at night.
When transitioning to nappy-free sleep, use a waterproof sheet to protect the mattress.
Bedwetting in Older Children and Teenagers
Older children and teenagers can also struggle with bedwetting. It’s important to reassure them that it isn’t their fault. A doctor can assess for underlying medical conditions and offer treatment options.
Now You Know How to Potty Train Your Child at Night
Hopefully, this guide has given you a clearer idea of how to approach nighttime potty training. While bedwetting can be distressing, using these strategies can help.
Take care,
Catherine x