Dealing with bedwetting, or nocturnal enuresis, is a common yet challenging issue for many families. It can be stressful for both the child and the parents. However, understanding the root causes and finding effective solutions can make a significant difference. In this guide, we'll explore various ways to tackle bedwetting, ensuring you have the tools to support your child through this phase.
Understanding and Addressing Your Child's Bedwetting
Bedwetting is often misunderstood, leading to unnecessary frustration. It's important to know that bedwetting is a normal developmental stage for many children. Factors such as constipation, infrequent drinking and voiding, genetics, hormonal imbalances, small bladder capacity, and stress can all contribute. Recognising that bedwetting is not a behavioural issue but a developmental one is key to providing the right support.
Interestingly, bedwetting often runs in families. If you or your partner experienced it as a child, your child might too. Hormonal factors can also play a role; some children develop the antidiuretic hormone (ADH) later, which helps reduce nighttime urine production. However, other factors should be considered, and hormones should not be the only focus. Sometimes, a small bladder capacity or underlying psychological factors like stress or anxiety can also be reasons for bedwetting.
Beyond these physical factors, it's crucial to consider the emotional impact. Children often feel embarrassed or ashamed about bedwetting, which can affect their self-esteem. As a parent, your understanding and reassurance can help mitigate these feelings, making the situation less distressing for your child. We have a few real-life stories on our website from adults who experienced bedwetting as children. Many were punished, which really knocked their self-esteem when, in reality, they were not in control of the bedwetting, and punishment only made things worse.
Preventative Measures for Bedwetting in Kids
Preventing bedwetting in your child involves a combination of practical strategies and lifestyle changes. Here are some tried-and-true tips that can help:
- Fluid Management: Try to limit your child’s fluid intake in the evening, especially caffeinated and sugary drinks. Encourage them to drink more water during the day to stay well-hydrated. Avoid giving them large amounts of fluid in the hours before bedtime. Milk, especially before bed, should ideally be avoided.
- Bathroom Routine: Establish a consistent bathroom routine by making sure your child uses the toilet before bed and first thing in the morning. Incorporating bathroom trips into their nightly routine ensures their bladder is empty before sleep. Sometimes, two trips to the toilet—one at the start of getting ready for bed and another just before sleep—can ensure the bladder is properly emptied.
- Bladder Training: Ensure your child is filling up and emptying their bladder frequently and not holding onto urine.
- Positive Reinforcement: Use a reward system for areas such as going to the toilet before bed and drinking enough during the day. However, it is best to avoid rewarding dry nights. Positive reinforcement can boost your child’s confidence and motivation.
Additionally, try to avoid giving your child large quantities of fluid close to bedtime and identify any bladder irritants in their diet, such as citrus fruits or chocolate, which can make the problem worse. By incorporating these strategies, you can help your child navigate and overcome bedwetting with confidence.
Medical Approaches to Address Bedwetting in Kids
Sometimes, the above strategies aren't enough. In such cases, medical interventions can be very effective. Here are a few options:
- Desmopressin: This medication mimics ADH (Anti-Diuretic Hormone), reducing urine production at night. It can be particularly useful for special occasions or as part of a longer-term strategy under medical supervision. This is something that will be prescribed by your GP if they have ruled out other factors or as a short-term solution for a sleepover.
- Alarm Therapy: Bedwetting alarms are designed to wake your child at the first sign of moisture, helping them learn to respond to the need to urinate. These alarms can be worn on pyjamas or placed under the sheets and have been shown to be highly effective in achieving dryness over time. The success of alarm therapy often depends on consistency and parental involvement in the process.
- Medications for Bladder Control: In some instances, doctors may prescribe medications to relax the bladder and reduce nighttime urination. These medications can help children who have overactive bladder muscles or small bladder capacity. As with any medication, it is crucial to discuss potential benefits and risks with a healthcare provider.
If your child is over the age of five in the UK, you can visit your GP for support. This guidance used to be for children aged seven but has more recently changed to age five to ensure that strategies to help bedwetting can be put in place sooner.
Practical Advice for Helping Kids Overcome Bedwetting
Supporting your child emotionally and practically is essential. Here are some tips:
- Patience and Reassurance: Let your child know that bedwetting is common and will eventually resolve. Consistent support and understanding can help reduce the child's anxiety and shame.
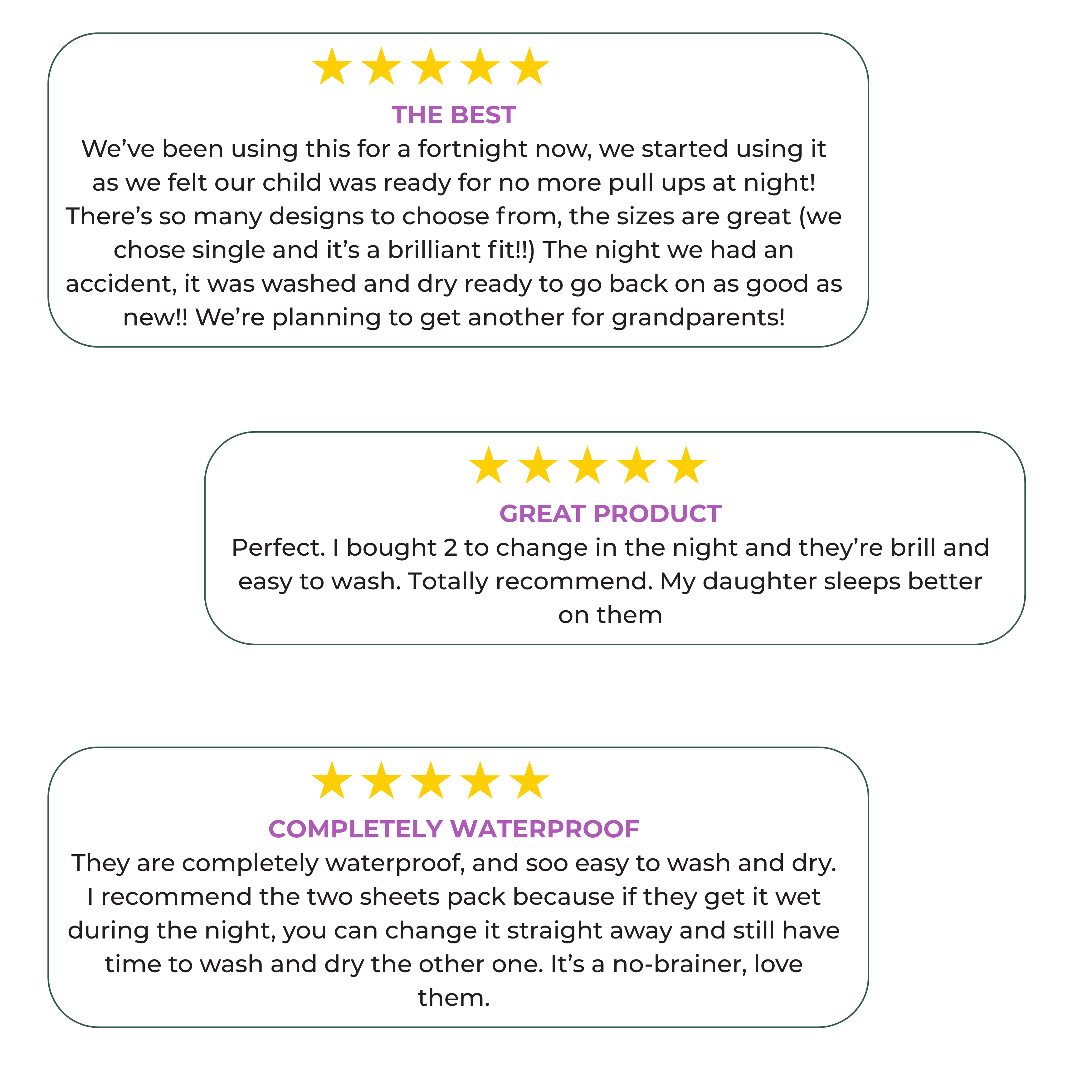
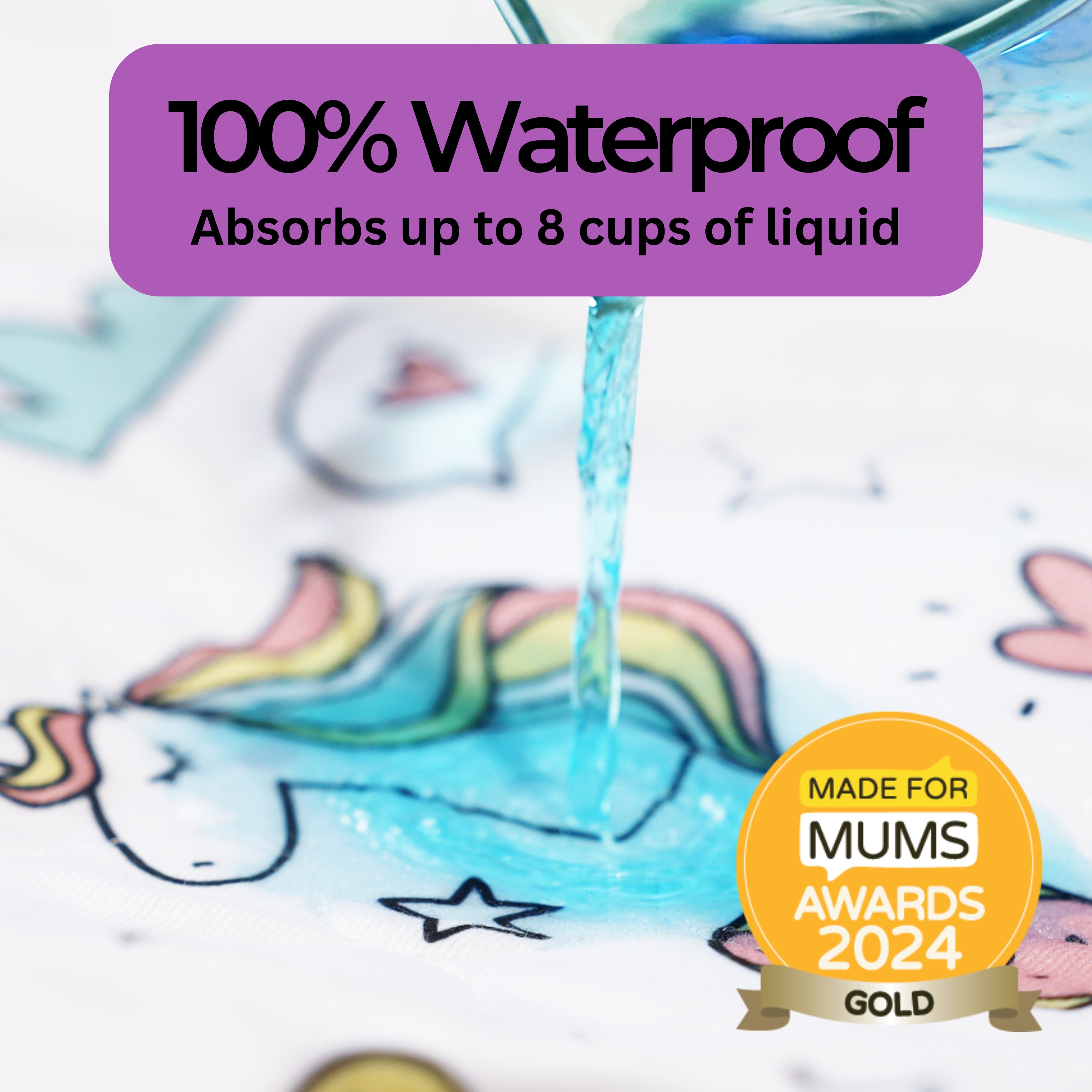
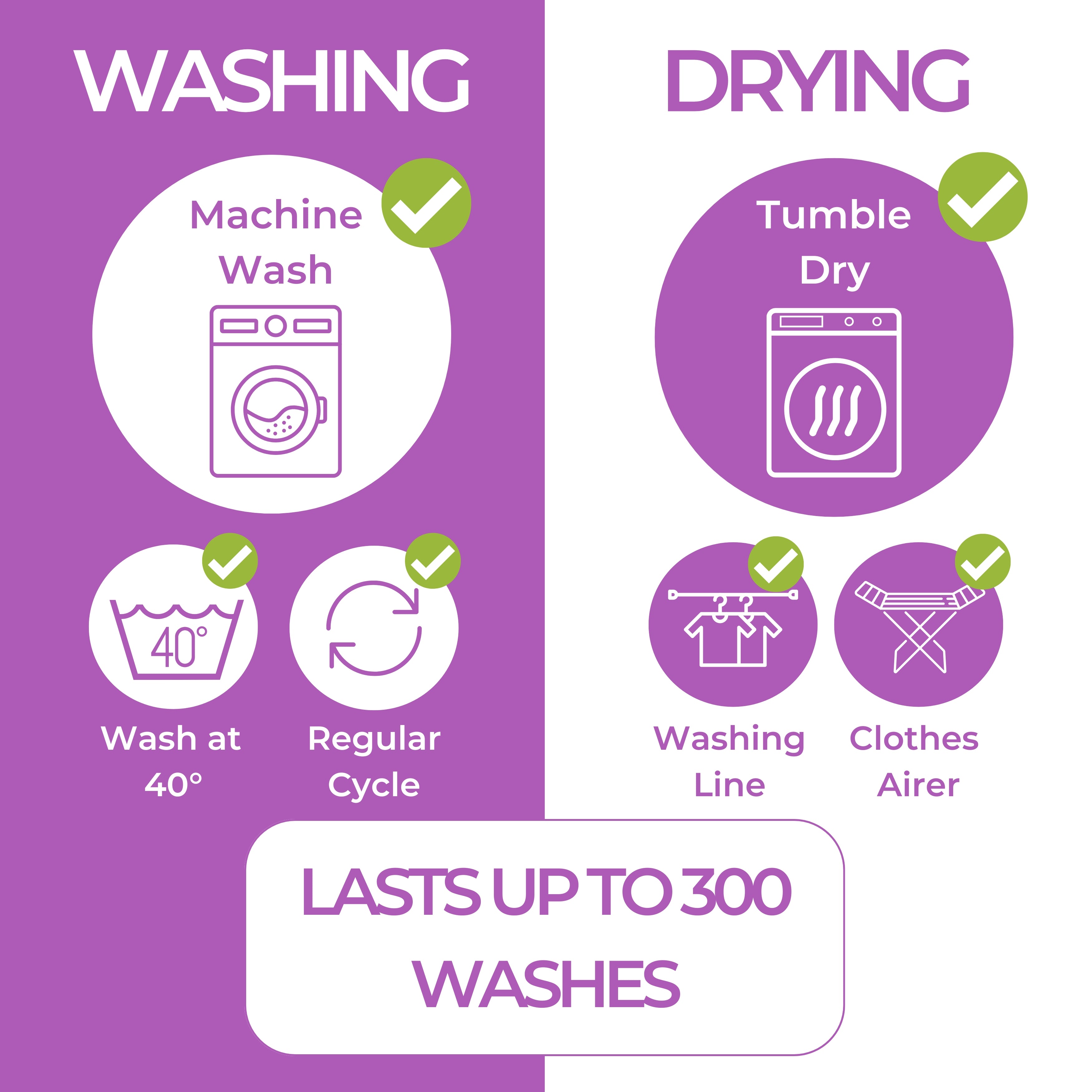
- Protective Bedding: Use waterproof mattress protectors like Hygge Sheets and have extra sheets and pyjamas ready to minimise the stress of nighttime accidents. Hygge Sheets are designed to provide a comfortable and effective barrier, making clean-up easier and ensuring your child gets a good night's sleep.
- Open Communication: Encourage your child to talk about their feelings. A safe, supportive environment can reduce anxiety and build trust.
- Avoid Punishment: Focus on positive reinforcement instead. Punishing a child for bedwetting can increase anxiety and exacerbate the problem.
Best Methods to Cure Bedwetting: What Actually Helps?
Finding the best cure for bedwetting often requires a combination of approaches tailored to your child's specific needs. Some of the most effective cures include:
- Consistency with Routine: Maintaining a consistent bedtime routine and bathroom schedule can significantly reduce bedwetting incidents.
-
Drinking and Toileting Frequency: Ensure that your child is drinking enough liquids during the day. The recommended daily intake of water for children is:
- 4 to 8 years old: 5 cups
- 9 to 13 years old: 5 to 6 cups
- 14 to 18 years old: 6 to 8 cups
- Parental Involvement: Active parental involvement in tracking progress and offering support can lead to better outcomes. Keeping a bedwetting diary can provide valuable insights into triggers and progress.
Ways to Support Your Child with Bedwetting Issues
- Empathy and Understanding: Ensure your child feels supported and not embarrassed.
- Professional Help: If bedwetting persists, consider seeking help from a paediatrician or a child psychologist.
- Educational Resources: Provide age-appropriate resources to help your child understand bedwetting.
- Support Groups: Connecting with other families experiencing the same issues can provide reassurance and advice.
Conclusion
Bedwetting is a common issue, but with the right understanding, strategies, and support, it can be effectively managed. Combining behavioural techniques, medical interventions, and emotional support can help your child overcome nighttime accidents with confidence. Remember, patience and consistency are key, and your child is not alone in this journey.
Take care,
Catherine x