Bed wetting in adulthood can be an overwhelming and often embarrassing experience. Whether it is due to incontinence, complications after surgery, or underlying medical conditions, it can have a significant impact on daily life and emotional wellbeing. According to the NHS there are an estimated 14 million people in the UK experiencing some form of bladder concern.
One medical condition that may contribute to nighttime accidents yet is not widely discussed is diabetes. Here we look into the connection between diabetes and bed wetting, why it happens, and what you can do to manage and reduce accidents.
The Link Between Diabetes and Bed Wetting
Diabetes affects how the body regulates blood sugar. When blood sugar levels are high, the kidneys work harder to filter and remove the excess glucose through urine. This increased urine production known as polyuria can lead to accidental urination during sleep. Bed wetting is commonly thought of as a childhood issue, but when diabetes affects bladder function, it can happen to adults as well and it’s more common than many realise.
Research suggests that adults living with diabetes may have up to a 70% greater risk of urinary incontinence compared with those without diabetes, which helps explain why nighttime wetting is not unusual in diabetic individuals. In fact, according to the National Association for Continence, up to 40% of females with diabetes experience urinary incontinence, highlighting just how strongly diabetes can impact bladder control.
For some adults, bed wetting can be one of the earliest indicators that diabetes may be present. When it occurs alongside symptoms such as extreme thirst, fatigue, blurry vision, or sudden weight changes, it can serve as an important signal that the body is struggling to regulate blood sugar. In these cases, seeking a medical evaluation promptly is vital, as early diagnosis and intervention can significantly reduce further complications and improve long term health outcomes.
Causes of Bed Wetting in Diabetic Patients
Several diabetes related factors can contribute to nighttime wetting:
-
Excess glucose causes increased urination
-
Nerve damage (diabetic neuropathy) can reduce bladder control
-
Overactive bladder due to weakened pelvic floor muscles
-
Sleep disruptions or deep sleep caused by exhaustion
-
Infections such as UTIs, which are more common in diabetics
It’s also important to recognise that bed wetting can occur even in adults who are managing diabetes well, everybody responds differently.
Managing Diabetes to Reduce Bed Wetting Incidences
Improving diabetes control can significantly reduce the risk of nighttime accidents. Maintaining stable blood sugar levels throughout the day plays a central role, as sudden spikes can increase urine production and put added strain on the bladder. Avoiding late night high sugar snacks and drinks can also help prevent glucose surges overnight. Some individuals may benefit from speaking with their healthcare professional about the timing of diabetes medications, as small adjustments can support better fluid and bladder regulation while asleep. Monitoring fluid intake throughout the day not by restricting water but by pacing it sensibly could also reduce the likelihood of nocturnal urgency. Lastly, if urinary tract infections develop, seeking prompt medical treatment is essential, as infections can worsen bladder sensitivity and contribute to bed wetting. Although medical care is fundamental, simple lifestyle changes can have a powerful and positive impact. Further advice and support can be found on the NHS website.
Exploring the Psychological Impacts of Bed Wetting
The emotional toll of adult bed wetting is often underestimated. Many individuals report feelings of shame or embarrassment, which can lead to strained relationships, avoidance of intimacy, or reluctance to sleep beside a partner. Sleep anxiety may develop over time, particularly for those who experience unpredictable or frequent nighttime accidents. Some people fear travelling, staying in hotels, or visiting friends because of uncertainty about managing their symptoms discreetly. These emotional responses are understandable and far more common than many people think, yet they deserve attention and compassion rather than silence. Opening up to a family member, loved one, medical professional or therapist can help. Reducing feelings of isolation and shame by replacing secrecy with support and understanding.
Preventive Measures for Bed Wetting
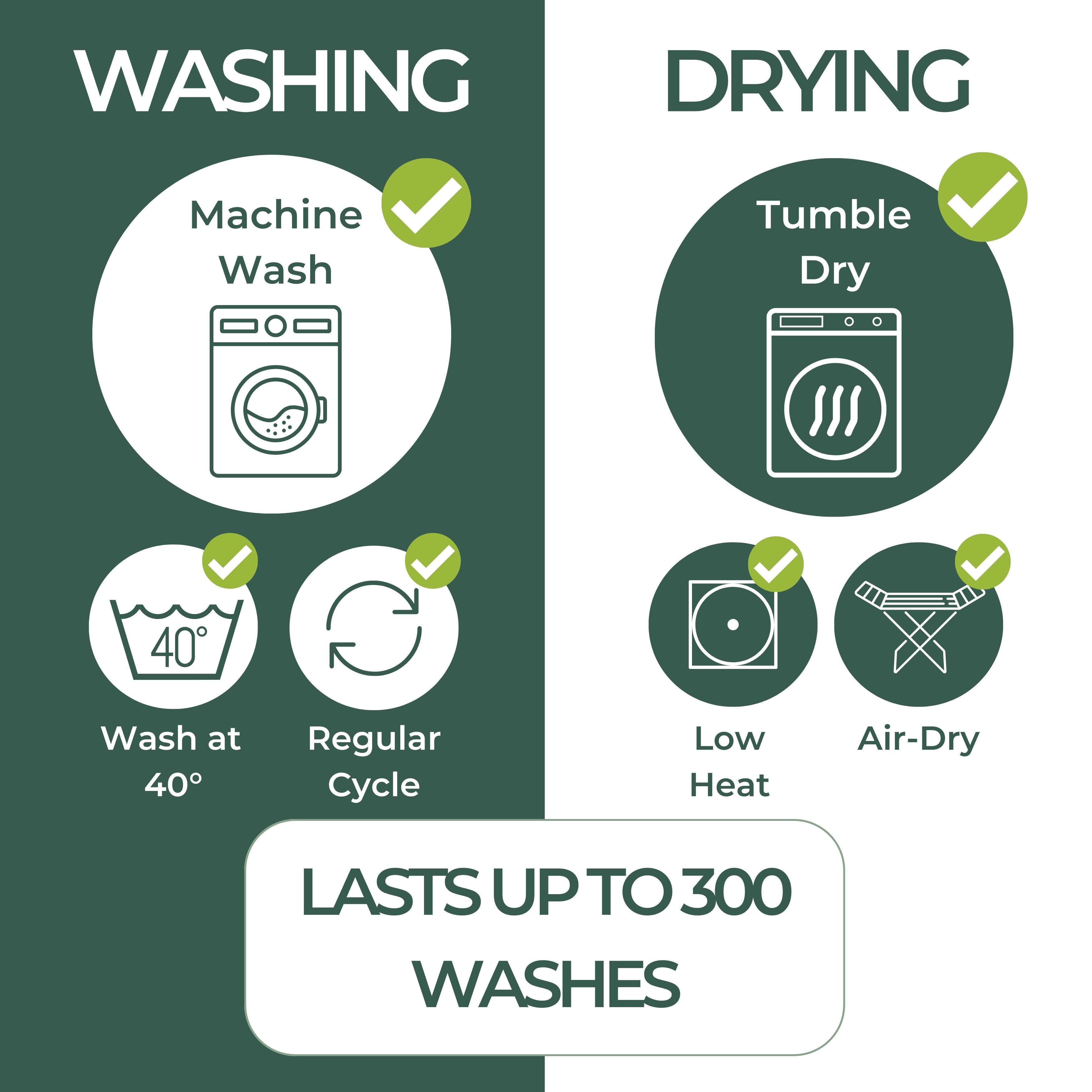
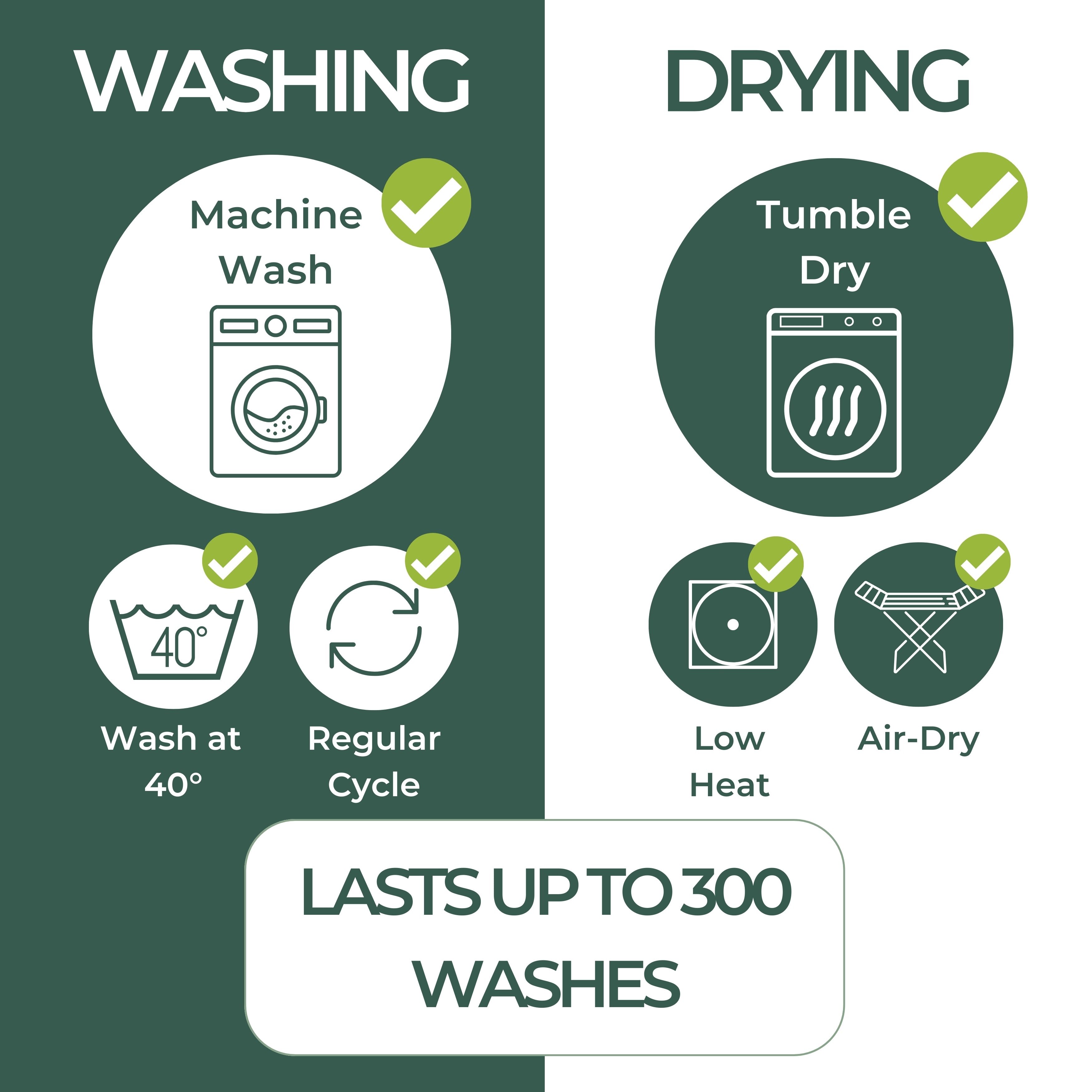
Alongside diabetes management, practical measures can help reduce the frequency of nighttime wetting and restore a greater sense of comfort and control. Waterproof bed pads or washable mattress protectors can reduce anxiety and make nights feel less stressful. Some people benefit from bladder training exercises or pelvic floor therapy to improve muscle strength and capacity. Others find that setting gentle nighttime reminders to visit the bathroom can prevent the bladder from becoming too full while asleep. Reducing caffeine, alcohol, and fizzy drinks particularly in the hours before bed can also lessen bladder irritation. While these solutions do not treat the underlying medical cause, they can significantly reduce stress and improve day to day confidence while longer term treatment is in progress.
Effective Treatment Plans
Treatment for diabetes related bed wetting varies from person to person and is usually most successful when tailored to the individual, but may include:
-
Adjusting diabetes medications
-
Treating bladder infections
-
Medication for overactive bladder or incontinence
-
Pelvic floor physiotherapy
-
Addressing neuropathy with proper medical management
Ultimately, many people find that a combined approach, medical support, lifestyle changes, and emotional care delivers the best outcomes.
Adult bed wetting is far more common than most people realise, especially among individuals managing diabetes and other medical conditions.It does not indicate failure or lack of control; it is a physical symptom that can be managed with the right support. With proactive medical care, lifestyle strategies, and emotional understanding, most people can significantly reduce or eliminate nighttime wetting episodes.